Understanding Male Factor Infertility: Causes, Diagnosis, and Treatment
Although many individuals and couples struggle with infertility, it is often mislabeled as a female reproductive condition. In reality, only 1/3 of infertility diagnoses are attributed to women. The other 2/3 are attributed to men, a combination of fertility challenges in both partners, or unknown causes. Once a physician determines male factor infertility may be complicating conception, a Semen Analysis (SA) is conducted as part of the Fertility Health Screening.
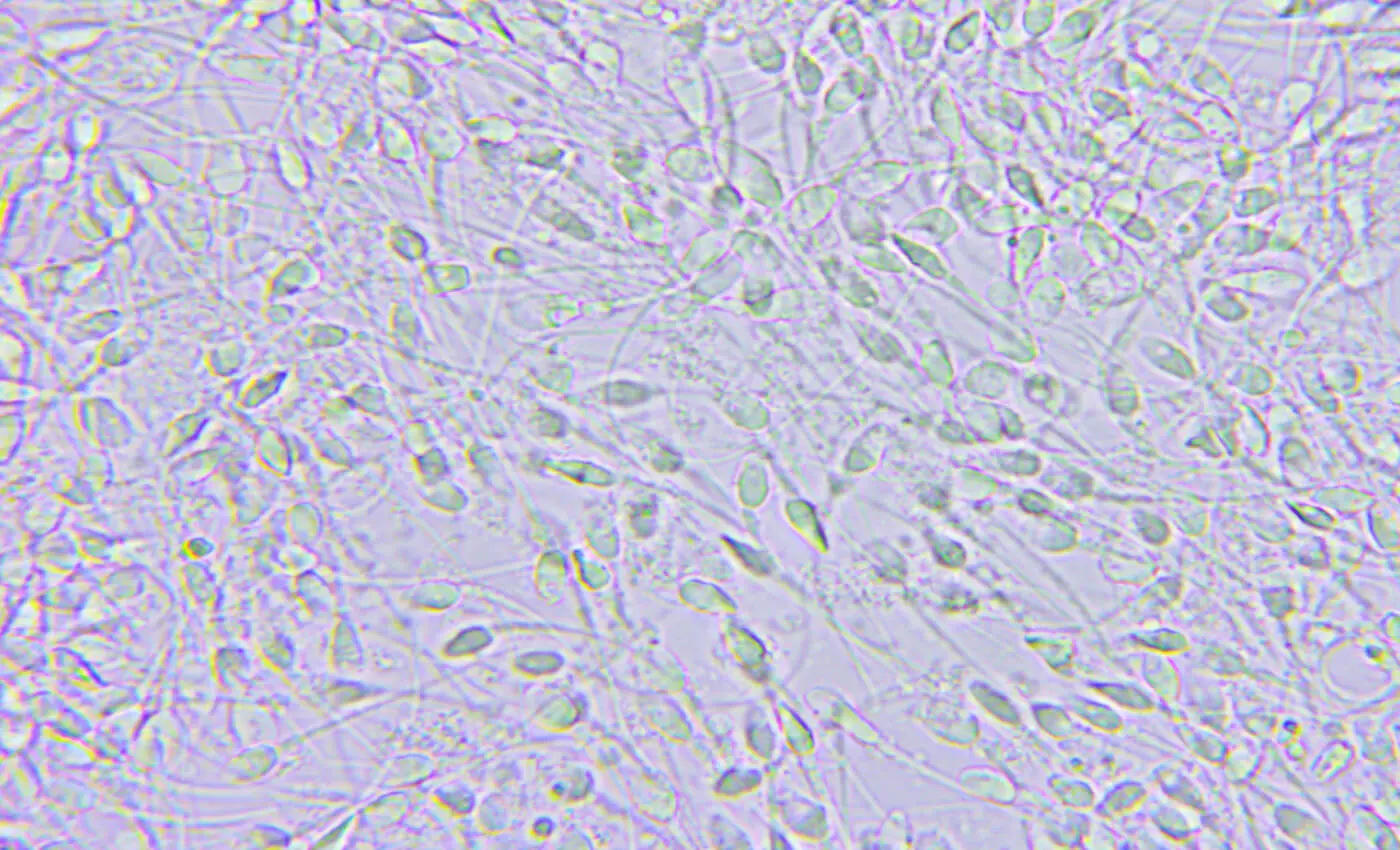
Semen Analysis
In order to diagnose male factor infertility, a semen analysis is conducted on a sperm specimen. At NYULFC, the semen analysis looks at three key metrics – sperm volume, sperm motility (movement) and sperm morphology (shape). Please be aware that there is a great deal of variability in sperm health and your physician may recommend testing twice prior to prescribing medical treatment.
Sperm Volume:Sperm volume or sperm count is seen as the most important factor in determining fertility in men. According to the World Health Organization[1], a total motile count of over 40 million is considered normal. Total motile count (the total number of sperm in a sample) is calculated by multiplying volume, motility, and count (per mL). Total motile count can be negatively impacted by a number of factors including: obesity, smoking, drug use, stress, exposure to toxins, injuries to the groin, overheating of the testes, hormone imbalances, anatomical issues, prior surgeries, and infections.
Many of the factors listed above may temporarily impact sperm volume, and may be corrected through lifestyle change or medical procedures. Prior to treatment, we encourage patients to speak with their physician to properly identify what may be causing low sperm count.
Sperm Motility: Sperm motility refers to the percentage of sperm that are swimming and how they are swimming (for example, are the sperm swimming in a circle or in a straight line?). According to the WHO[1], a motility rate greater than 50% is considered adequate. Sperm motility is impacted by a variety of factors, and two samples may be required in order to determine the cause and course of treatment. Some factors that impact sperm motility include: obesity, exposure to chemicals, injury to the pelvic area, smoking, poor diet, varicoceles (enlarged veins inside the scrotum that cause an increase in temperature), fevers, genetic disorders, ejaculatory frequency, and using lubricant while producing a sample.
Sperm Morphology: Occasionally, a semen analysis will examine the shape of the sperm (morphology). While this metric is not used to calculate the total motile count, morphology can be important for fertility as sperm must have a specific shape in order to successfully reach and penetrate an egg. For patients diagnosed with low sperm morphology, there is good news – having low morphology has not been shown to result in birth defects, but it may take longer to naturally conceive or assisted reproductive technologies like In Vitro Fertilization may be necessary. Some potential causes of poor or abnormal sperm morphology include: using lubricant while producing a sample, variability in testing, sexually transmitted infections, genetic abnormalities, and chemical exposures.
Treatment for Male Factor Infertility
Based on the results of one or two semen analyses, a NYU Langone Fertility Center physician will be able to determine if sperm health is impacting fertility and diagnose male factor infertility. At NYU Langone Fertility Center, we pride ourselves on providing patients with individualized treatment options and exceptional clinical care, and treating male factor infertility is no exception. As a first step, lifestyle measures may be recommended to encourage healthy sperm development and improve fertility. These include: no smoking, maintaining a healthy weight, limiting the consumption of alcohol, eating healthy foods like fruits and vegetables, cardiovascular exercise, consistent sleep of more than 6 hours per night, choosing boxers instead of briefs, lowering stress levels, avoiding extreme heat (hot tubs, steam rooms, saunas, etc.).
It takes sperm 72 days to reach maturity inside the body, so if the above measures do not improve fertility in a few months, clinical action may be necessary. In some cases, a NYU Langone Fertility Center doctor will refer patients to an andrologist specializing in male factor infertility for treatment.
Fertility treatment options for male factor infertility include:
- IUI (intrauterine insemination): For cases in which there is mild, unexplained low sperm count, an IUI may be performed in order to increase the chances of conception. Sperm is processed and placed in the female partner’s uterus during ovulation, increasing the odds that a healthy sperm will reach an egg.
- In Vitro Fertilization: For moderate male factor infertility, In Vitro Fertilization (IVF) may be recommended to create embryos. In IVF, sperm is placed alongside an egg in a culture dish and transferred to an incubator where fertilization occurs naturally.
- In Vitro Fertilization with ICSI (Intracytoplasmic Sperm Injection): For moderate to severe male factor infertility, IVF with ICSI may be advised to produce an embryo. In these cycles, our embryologists can utilize intracytoplasmic sperm injection ("ICSI") to inject a single sperm directly into each egg. If a sperm sample is considered 'borderline,' some eggs may be injected while others are given the chance to fertilize naturally in the petri dish.
- Surgery: in cases where an anatomical obstruction is preventing the production of healthy sperm, surgery may be required to correct the problem. Surgery is usually minimally invasive and patients can typically return home the same day.
- Medication: in some cases, hormonal medication may be prescribed to improve sperm production or antibiotic medication may be prescribed to treat infection that may be impacting sperm production.
Interested in learning more? Reserve a consult with one of our physicians to learn more about male factor infertility. We’re here to go at your pace and answer any questions you may have as you become educated about your options. Whenever you’re ready, we’ll be right here.
[1] Cooper, Trevor G et al. “World Health Organization reference values for human semen characteristics.” Human reproduction update vol. 16,3 (2010): 231-45. doi:10.1093/humupd/dmp048
Categories
The NYU Langone Fertility Center Blog
At NYU Langone Fertility Center, our first job is to support our patients as they become educated about their reproductive health and fertility treatment options. Our blog connects patients with the most up-to-date information, technologies, and insights into fertility care. From egg freezing to IVF to third-party reproduction options, we explore every facet of assisted reproductive technology and empower patients with the knowledge they need to navigate their family building journeys.

